England's Maternal Mental Health Services (MMHS) - not to be confused with Specialist Perinatal Mental Health Services (SPMHS) - provide lifesaving and life-changing care for women experiencing moderate mental illness directly linked to their maternity experience.
MMHS were introduced to fill a gap between specialist perinatal mental health teams and services supporting more common perinatal mental health problems (e.g. NHS talking therapies).
The Maternal Mental Health Alliance's research on the current state of MMHS in England, for the first time, maps where these services are and which care pathways are offered:
Last updated: September 2024
Download full reportMMHS have started delivering life-changing care, but they are small services. To ensure more women, babies and families can access support, further action is required:
Ongoing targets for MMHS are needed as the current commitments have not yet delivered the mental health care women and birthing people and their families need.
Given it is not ‘job done’, continued focus from the government and NHS England is required, as well as clear expectations for all local areas of what the MMHS offer should be.
Download the reportFurther resources are required so all MMHS can deliver care across all the required pathways, including equipping every MMHS to provide a pathway for women whose babies have been removed due to safeguarding concerns.
The current variability in care across different parts of the country, means existing levels of funding are not enough. A clear timeframe showing how teams will be supported to deliver care across all pathways is urgently needed.
Download the reportIf we want to see changes in the current trends of negative outcomes for certain groups of women and birthing people, it’s crucial that MMHS are resourced to reach out, become more culturally inclusive and adapt to the unique needs of their diverse local communities. The voices of those with lived experience must be included in service design.
Download the reportImproving the quality of the data being collected to identify inequalities in prevalence, experience and outcomes in maternal mental health could help ensure services meet the needs of ALL women and birthing people and their families.
The link between better data quality and improvements in care needs to be made clear to staff who face many pressures on their time.
Download the reportOur data shows variation between MMHS in referral criteria, assessment methods and psychological therapies offered. Quality standards exist for specialist perinatal mental health services where they have helped determine basic levels of care and raise standards.
Having such guidance for MMHS would ensure there are baselines so that all women, babies and families accessing these services receive compassionate and equitable treatment regardless of where they live.
Download the reportFor healthcare professionals to effectively support women in the perinatal period they need to be able to access education, including training on maternal mental health and trauma. MMHS can play an important role in delivering this training, if they are given allocated time to provide this.
In addition, all services working with women and birthing people during pregnancy and after birth must have knowledge of their local MMHS, so that women who need this specialist support can be appropriately referred and women, babies and families can access care as quickly as possible.
Download the report Maternal Mental Health Services (MMHS) | Specialist Perinatal Mental Health Services (SPMHS) |
| For women with moderate – severe mental health conditions stemming directly from their maternity experiences | For women with complex mental health conditions before, during and after pregnancy |
| Offer evidence based psychological interventions | Psychiatry-led multidisciplinary teams, also including specialist mental health nurses, psychologists, health visitors, social workers and others |
| Can provide inpatient treatment where required in a mother and baby unit |
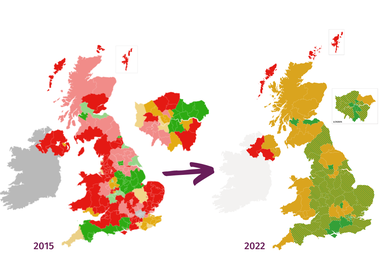
Specialist services are foundational for perinatal mental health care. Our maps show where these services are and aren't available in the UK.
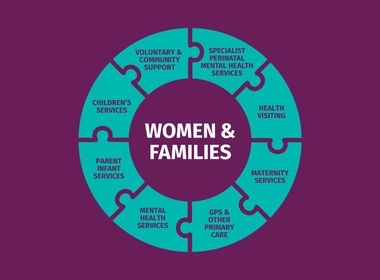
Women and families across the UK need equal access to high-quality, compassionate care and support, including and beyond specialist services.

Let's come together and make sure maternal mental health is a priority for the government!