Posted By: Amy Tubb
4th June 2025
2 minute read
Members of the Maternal Mental Health Alliance (MMHA) in Northern Ireland, including Action on Postpartum Psychosis, Aware NI and The BPS, are deeply concerned by a recent story shared by Shelley Browne, a mother separated from her newborn baby and admitted to a general psychiatric hospital for five weeks.
Shelley’s experience, featured by BBC One Northern Ireland’s ‘Spotlight: Mums in Crisis’, is a heartbreaking reminder of the urgent need for a Mother and Baby Unit (MBU) in Northern Ireland.
The BBC programme also highlighted the tragic case of Orlaith Quinn, a mother who died by suicide in 2018 less than two days after the birth of her third baby. Following her death, which an inquest found “foreseeable and preventable”, a recommendation was made to establish an MBU in NI.
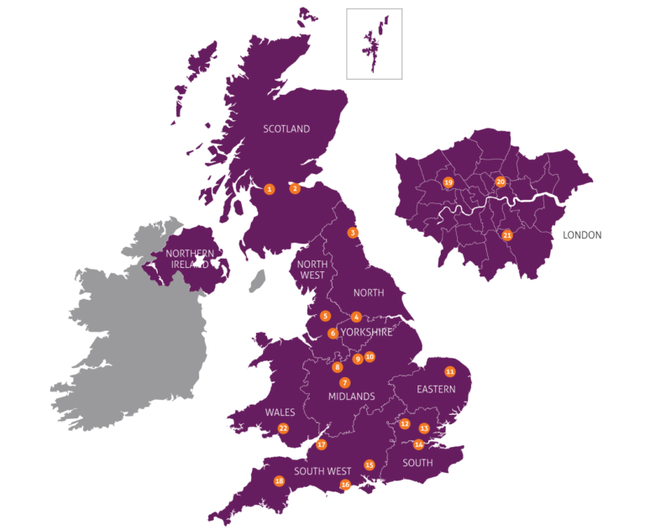
Despite cross-party support and Belfast Trust agreeing to host the MBU, the business case remains significantly overdue, with no funding yet identified. While some positive and welcome interim measures have been implemented, elsewhere in the UK, temporary units were established to address the urgent need to provide specialist inpatient perinatal mental health care. Northern Ireland has yet to take similar action.
While we remain cautious about short-term interim units becoming a "good enough" long-term solution, it’s clear that action is needed now to prevent further trauma and loss of life. The Exeter MBU, featured in last night's programme, shows how a temporary unit, though not perfect, can provide safe, specialist care that keeps mums and babies together during recovery as plans for a permanent facility progress.
When I was admitted, I was told that no babies were allowed in. This was extremely distressing. In hospital, I was diagnosed with postnatal depression and “disassociation”. I now believe I was experiencing postpartum psychosis, but without specialist perinatal mental health services, this wasn’t even mentioned to me.
Alex, MMHA Lived Experience Champion
Read more about AlexThe evidence is clear: MBUs save lives and improve outcomes for mums and babies. These specialist facilities allow mothers to receive expert psychiatric care while continuing to nurture their bond with their baby in a secure and supportive environment. Instead, women, babies, and families in Northern Ireland are being let down compared to the rest of the UK.
"Today we heard from mums and their families who urgently need better mental health care. It’s a story APP hears all the time from the mums who attend our postpartum psychosis Northern Ireland peer support group who, like Shelley, have been separated from their babies and admitted to psychiatric inpatient wards for treatment. We need dedicated funding and we need firm deadlines so that this Mother and Baby Unit in Belfast can be built and opened as soon as possible." Dr Jess Heron, Chief Executive
No mother should have to choose between her mental health and staying with her baby. The lack of a Mother and Baby Unit in Northern Ireland is a glaring gap in our care system, and one that continues to harm families. AWARE NI stands with every woman calling for urgent action. The time for delay is over.
The powerful lived experiences of mums such as Shelley who bravely shared their stories can no longer continue to be ignored. NI continues to be the only UK nation without a MBU despite tireless campaigning for over 20 years and cross party agreement for the need for such a facility. We urge the Department of Health to advise on the Business Case and secure capital and revenue funding as a priority. Mothers and their babies in NI deserve better.
It is deeply concerning that Northern Ireland remains the only part of the UK without a specialist Mother and Baby Unit, forcing mothers experiencing mental health challenges to be separated from their babies in general psychiatric wards. This lack of specialist care puts immense emotional strain on families during a critical period for bonding and recovery. The Department of Health must make the development of a dedicated Mother and Baby Unit an urgent priority. This service is not only long overdue—it is essential. The time for action is now.
"Given all that we know about the importance of the first 1001 days for future emotional and developmental growth we should not be in the situation as a country where we are separating mums and babies due to funding A mother and baby unit should be made a funding priority to ensure that more mums and babies don’t have to suffer. This is early intervention in its most important form for mother and baby." Tracey Ripley-McElvogue, Project Co-ordinator, East Belfast Sure Start
Find out more about the Stronger from the Start Infant Mental Health Alliance
At Support 2gether, we walk beside mothers who become mentally unwell during and after pregnancy. Some experience such profound distress that they require hospitalisation — and far too often, this means being separated from their babies.
Northern Ireland remains without a Mother and Baby Unit. This is not just a gap — it's a crisis.
We know, firsthand, how quickly a mother can spiral in the absence of the right care. And we know the devastating impact of separating mother from baby during this vulnerable time.
Our health system is not equipped to meet the needs of these mothers. Specialist, compassionate, and immediate care is not a luxury — it’s a lifeline.
We are calling for urgent action.
The long-overdue Mother and Baby Unit in Northern Ireland must become a priority. No more delays. No more excuses.
Because mothers deserve to recover with their babies by their side.
Because early intervention saves lives.
Because every mother matters.
"Shelley’s story is not unique in Northern Ireland. Her generosity and courage to tell it in this way is and stands as a remarkable challenge to the stigma that many women, and birthing people, along with their babies and families face during an acute mental health crisis in the perinatal period. Why does Northern Ireland continue to lag behind the rest of the UK in providing services that not only make health economic sense but give families in a mental health emergency all the psychological safety and treatment a MBU can offer? Our local strategy is clear about the need and its framework for delivery. The funding commitment is available. The workforce is ready and the families are so worthy. Let’s get on with it." Professor Michele Kavanagh,Consultant Clinical Psychologist, Co-Chair BPS Faculty for Perinatal Psychology UK, DCP NI Network Member
"The Division of Clinical Psychology in NI appreciates Shelley’s courage in sharing her story and alongside colleagues calls for the provision of a regional Mother & Baby Unit. Mothers and babies in Northern Ireland have the right to expect equity of care in being able to access the same services available across the rest of the UK. We also call for investment in Psychology services across all Maternity Units as highlighted in the RQIA Review 2017 Recommendation 1. Early support and Intervention is crucial in helping to prevent further distress and impact on mothers and families." Dr Sarah Meekin, Chair for Division of Clinical Psychology NI, Head of Psychological Services, Belfast Health & Social care Trust
Learn more about BPS and the Division of Clinical Psychology NI
Having no mother and baby unit in NI reinforces stigma and fear. This campaign has gone on too long and as we speak more mums and babies are continuing to be harmed by the inappropriate care that we saw and heard on the Spotlight programme. We need urgent action and funding without any further delay.
It was time to act nearly 20 years ago when an MBU was first discussed. Women, babies, and families can’t wait any longer for this lifesaving care.
The business case is on the table. The need is overwhelming. The political will must now follow. Funding must be found without further delay. Mothers and babies in Northern Ireland deserve better.
Ms Sinéad McLaughlin, SDLP MLA for Foyle