Posted By: MMHA
1st July 2023
4 minute read
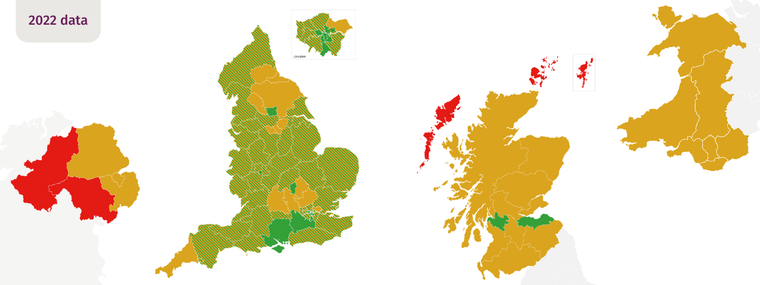
The MMHA’s latest report on specialist perinatal mental health (PMH) community services in the UK highlights the significant progress made in all four nations since 2013. However, access to life-saving mental healthcare for pregnant women and new mothers remains uneven, with many regions still lacking the necessary resources. Mental health-related deaths during pregnancy or up to six weeks after birth are increasing, emphasising the urgency of addressing this issue.
The MMHA’s Freedom of Information (FOI) request on budget allocation and spending on services found that although 89% of the 70 areas that responded had seen their budget increase from 2020/1 to 2022/3, 66% indicated there would be an underspend for 2022/3. Workforce-related issues were the most frequently cited reason for underspending (58% of respondents), but many teams provided evidence indicating this was due to unclear or late budget allocation, with no guarantee of continuation. This is inevitably resulting in women, babies, and families not receiving the care they need.
One healthcare professional told the MMHA: “We have had no increase in funding since inception of service. Despite our understanding that this should be ringfenced commissioners and managers have spent this money elsewhere. We have protested but with no effect. Nonetheless, the expectation that we see more women each year (in line with trajectories as if funding had filtered down) continues. We are working far beyond funded capacity which – as predicted and highlighted repeatedly – is now manifesting as increased sickness, stress, burnout and increased staff turnover.”
Secure funding is vital for maintaining and building upon the progress made with the expansion of specialist PMH services. Without it, recruitment will be impacted, exacerbating existing problems of understaffing and low morale, and ultimately specialist services may struggle to deliver urgent and necessary care to women who desperately need it. To break this cycle, teams must be shown that there is secure funding available.
MMHA President, Consultant Perinatal Psychiatrist Dr Alain Gregoire said: “Over the last ten years, there has been a growing understanding of the importance of specialist care for maternal mental health, which has led to welcome improvements across the UK. However, it’s crucial that this momentum and commitment is maintained. National and local decision-makers must ensure that allocated resources reach clinical services to ensure that mothers, babies, and families can access the care they need. We must grasp this exceptional opportunity to make a real and lasting impact on the lives of women, babies, and future generations.”
In addition to detailed area maps and analysis of FOI data, the MMHA’s report features recommendations that aim to enhance the accessibility and quality of specialist PMH services, as well as broader care for women, babies, and families impacted by PMH problems.
Eleanor, a mum from Bromley, said:
“When I realised that what I was experiencing wasn’t just “the baby blues” I reached out to my mental health midwife and was referred to my local perinatal mental health team. It was invaluable being under their care. Thanks to the support I received, my bond with my daughter is so strong now and I’m really enjoying being a mum. Every family should have access to the same care if they need it.”
The MMHA is a charity and network of over 120 organisations dedicated to ensuring all women and families impacted by perinatal mental health problems have access to high-quality, compassionate care and support. We bring the maternal mental health community together and make change happen by combining the power of real-life experience with clinical and professional expertise.
Contact: amyt@maternalmentalhealthalliance.org | 0207 117 2875